Companies are more willing to consider covering weight-loss drugs
Nearly one in four employers say they are either somewhat or very likely to begin covering the cost of anti-obesity medications within the next year.
That’s according to a new Employer Health Benefits Survey from KFF (formerly the Kaiser Family Foundation). But while a growing number say they’re open to covering GLP-1 drugs, they’re still in the minority. Some 62% of the firms surveyed said they are “not likely” to begin coverage in the coming year.
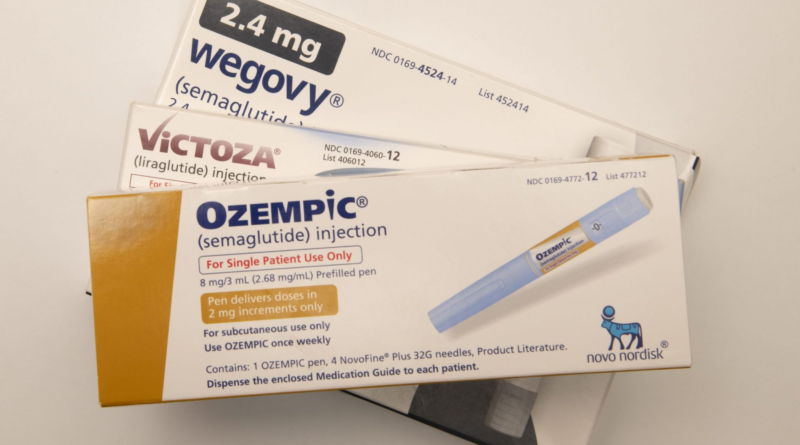
A lot of the reason for the hesitation is cost. The list price for Wegovy is $1,350 for a four-week supply. Ozempic is in the same neighborhood. Among companies that do provide coverage, 46% say the decision “will have a ‘significant impact’ on their prescription drug spending,” writes KFF.
Larger companies were more likely to cover the expense than smaller ones.
Another part of the hesitation is the length of time the drugs would be used. Several companies that cover them now also require workers to enroll in a lifestyle or weight-loss program in hopes of eliminating the need for these meds over time.
“Coverage for these drugs is likely to remain a hot future topic as employers and other payers gain insights about the long-term effectiveness and costs associated with these drugs,” writes KFF. “A key issue for payers and users of these medications is whether those who use them can eventually maintain lower weights without continued reliance on these medications.”
Ironically, the increase in the number of firms considering coverage of GLP-1 drugs comes as a new survey finds that the majority of Americans who are hoping to lose weight don’t want to do so using these drugs.
A survey of 2,200 adults by the nonprofit Physicians Committee for Responsible Medicine found that 62% said they would favor a diet change over taking an injectable weight-loss drug.
The Broadsheet: Covers the trends and issues impacting women in and out of the workplace and the women transforming the future of business.
Sign up here.